Use of CPAP in recovery shows potential to reduce ICU post operative admissions

In a trial at Our Lady of Lourdes Hospital, Drogheda, consultant anaesthetist Dr Jubil Thomas, demonstrated the ability of High Flow Oxygen Therapy (HFOT) and Continuous Positive Airway Pressure (CPAP) to adequately oxygenate patients both pre and post operatively, with the potential to improve throughput within the theatres and reduce post operative ICU admissions.
The use of High Flow Oxygen Therapy (HFOT) is increasing both for Preoxygenation and Apnoeic Ventilation (particularly for ENT cases), but also for difficult airway management and Rapid Sequence Induction (RSI). Several devices exist for the provision of HFOT however, a device which delivers only HFOT has limitations. A device which can also provide CPAP has additional benefits such as the ability to follow the patient throughout the peri-operative setting and the option to escalate therapy.
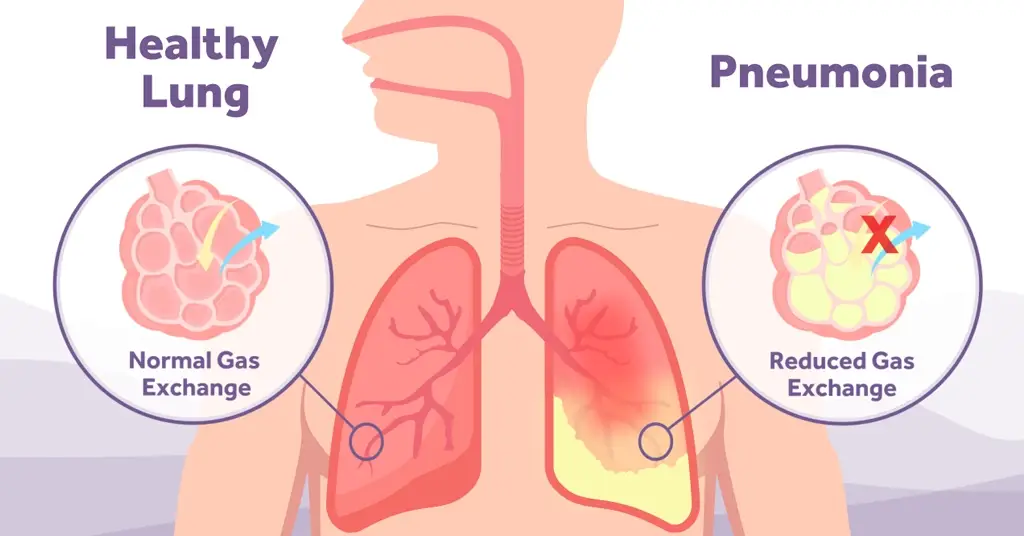
Firstly, in pre-op to provide pre-oxygenation for high-risk patients, some studies have reported an association between severe obesity and difficult intubation, male patients with severe obesity, especially ones with BMI more than 50 and obstructive sleep apnoea (OSA), as well as patients with a neck circumference > 42 cm had a higher risk of difficult mask ventilation and intubation [1]. Enhanced Recovery after Surgery (ERAS) suggest the use of high flow should be considered as an adjunct during mask ventilation in patients with a suspected or known difficult intubation. This has been demonstrated to help maintain oxygenation by increasing apnoea time up to 40% and can reduce peri-intubation desaturation during anaesthesia induction [2].
Following on from surgery the patient can transition with ease onto CPAP which is beneficial for bariatric patients as they can develop increased work of breathing as well as higher risk of perioperative atelectasis persisting for longer duration compared to patients with normal [2] weight. These patients can often remain longer in recovery and the potential to deliver CPAP quickly may well shorten their time in recovery thus assisting with the patient throughput in the Operating Room.
In the UK, one in three people who access the health service have two or more chronic conditions and one in three adults admitted to hospital as an emergency in the UK have five or more comorbidities [3]. Comorbidities are more frequent in the obese population, including those requiring surgical intervention. It is estimated that approximately 30% of the general surgical population present with obesity [4].
It is therefore fair to assume that hospitals are operating on more patients classed as clinically obese with increased likelihood of obstructed airways and complications both during surgery and recovery. The World Health Organisation Regional Obesity Report 2022 estimated that 26% of the population in Ireland and 28% in the UK [5] are obese, with a BMI over 30. As patients presenting for surgery become more complex, the use of heated humidified therapies such as HFOT and CPAP during recovery is becoming more common.
Our Lady of Lourdes Hospital in Drogheda is finding the number of patients undergoing ENT surgeries with significant comorbidities is increasing. They are operating on more patients classed as clinically obese with increased likely hood of obstructed airways and complications both during surgery and recovery.
A recent case study at Our Lady of Lourdes Hospital illustrates how using CPAP in recovery can [6]:
- Help with the recovery of complex high BMI patients
- Avoid recovery delays
- Avoid ICU escalations
- Reduce HDU admissions and lessen time spent in HDU if admission is required.
The Patient
50 years
BMI >30
Smoker
COPD
Obstructive Sleep Apnoea (OSA) – Nocturnal CPAP
Procedure
Septoplasty – deemed suitable for the procedure as DOSA and overnight stay.
Surgical plan – was Septoplasty with placement Nasal splints with pack.
Anaesthetic plan – was pre oxygenation by HFOT using Aquavent FD140i and postop extubate onto CPAP by face mask on the same equipment.
Pre-operatively the patients baseline oxygen saturation was 93% on Room air.
Intra-operatively
After intubation the patient’s oxygen requirements were significantly high.
FiO2 75%
peep 12
SaO2 88% – 92% and
PO2 7.8 KPa on ABG
The plan was therefore to attempt extubation on to CPAP via face mask. Postoperatively the patient was extubated on to CPAP via face mask with 60% oxygen which was weaned down over the next hour. The patient was transferred to HDU for overnight observation where they continued to improve and were deemed stable to be discharged later that night.
The patient had a history of Obstructive Sleep Apnoea, OSA which is a common condition among patients with severe obesity, it is associated with increased risk of cardiopulmonary events and a significant mortality rate. ERAS in their 2021 guidelines for perioperative care in bariatric surgery recommend that patients with OSA on home CPAP therapy should use this in the immediate post operative period and patients with obesity hypoventilation syndrome (OHS) are at higher risk of respiratory adverse events [2].
Post operative NIV should be considered liberally during the immediate post operative period, particularly in the presence of hypoxemia. The use of CPAP/BiPAP treatment, when necessary, can decrease the risk of cardiopulmonary complications in patients with OSA who undergo surgery [2].
While this patient was transferred to the HDU for after care, such was their improvement that they were discharged without the requirement for a costly overnight stay and ensured a HDU bed was available for the next patient. It is reasonable to think that the early intervention post operatively with CPAP played a part in the faster recovery of the patient and the subsequent freeing up of the HDU bedspace.
[1] Moon TS, Fox PE, Somasundaram A et al (2019) The influence of morbid obesity on difficult intubation and difficult mask ventilation. J Anesth 33(1):96–102 The influence of morbid obesity on difficult intubation and difficult mask ventilation – PubMed (nih.gov)
[2] Stenberg, E., dos Reis Falcão, L.F., O’Kane, M. et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: A 2021 Update. World J Surg 46, 729–751 (2022). https://doi.org/10.1007/s00268-021-06394-9 Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: A 2021 Update | SpringerLink
[3] Dr Asangaedem Akpan, Dr Kieran Walsh, The Impact of comorbidities on health services, BMJ Best Practice, 29 March 2021
[4] Andrea P Haren, Shrijit Nair, Maria C Pace, Pasquale Sansone, Intraoperative Monitoring of the Obese Patient Undergoing Surgery: A Narrative Review, Advances in Therapy, 5 June 2021.
[5] World Health Organization. Regional Office for Europe. (2022). WHO European Regional Obesity Report 2022. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/353747
[6] Data on File, Armstrong Medical Ltd