The Mucociliary Escalator

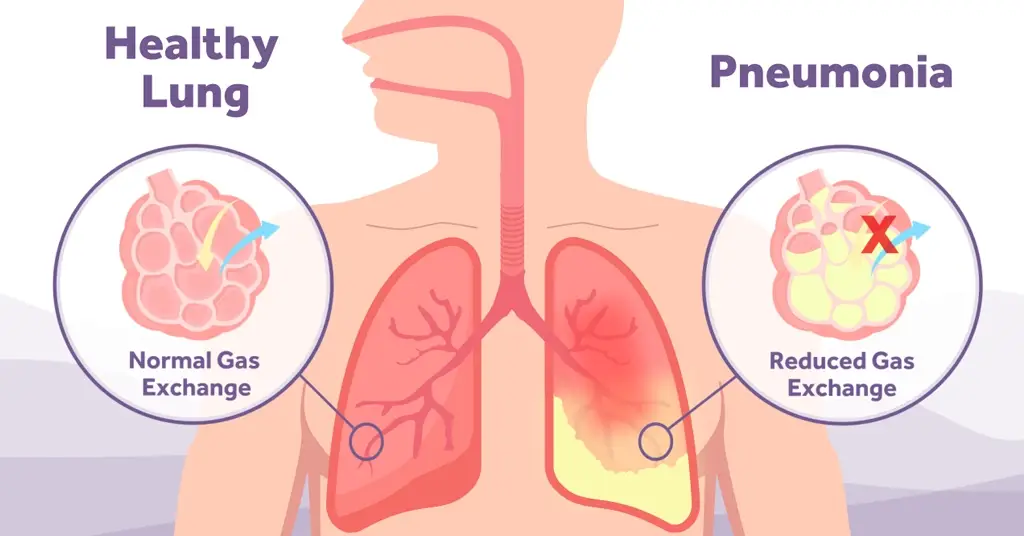
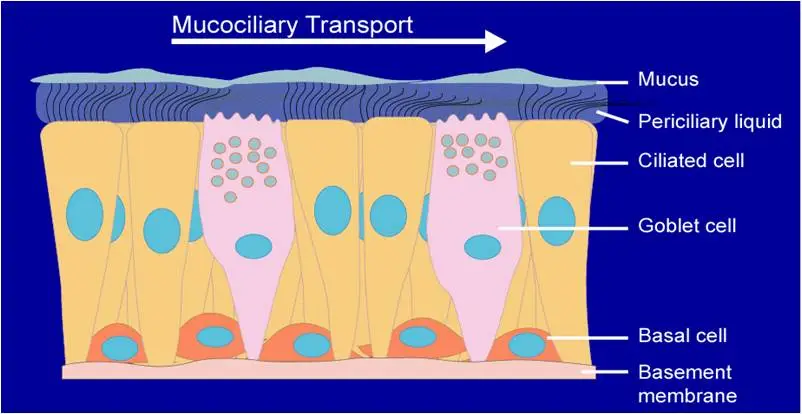
The “Mucociliary Escalator” is an integral part of your body’s host defence system. Mucus provides an anatomical barrier for pathogens and irritants, catching them before they can penetrate the delicate lung epithelium and cause damage. An effective mucociliary escalator will transport mucus, with any captured foreign particles, in an upstream direction towards the upper airway away from the alveoli. At this point a cough or throat clearing reflex is initiated and the mucus is expelled from the respiratory tract. Mucus is either then swallowed, with stomach acid killing trapped pathogens, or expectorated.
An effective Mucociliary Escalator is dependent on;
Integrity and function of the ciliated epithelium
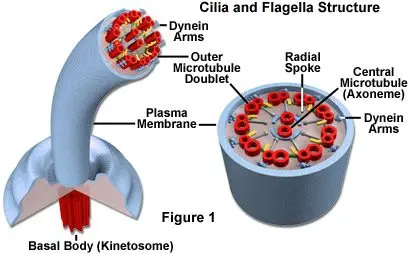
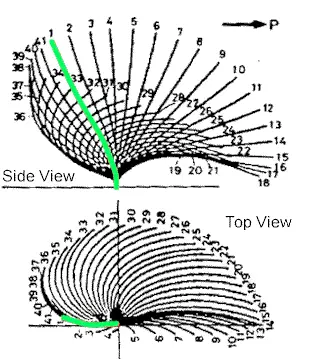
The lung epithelium is described as “ciliated” meaning that the upper surface of each epithelial cell is covered in Microvilli Cilia, or tiny cellular hairs. Each cilium is formed of microtubules held together with radial spokes and dynein arms (see fig.2). This complex internal structure allows the cilia to bend and beat in a distinct pattern. Initially, reviews on animal studies showed that this is a forward “power stroke” and then a “recovery stroke” which is back and round to the side (see video in fig.3). With the advent of digital high speed imaging it has been possible to show that respiratory cilia beat forward and backwards within the same plane without a classical sideways recovery sweep.
Human respiratory cilia beat with a frequency between 12–15 Hz in the nose and major airways. To facilitate mucus clearance, respiratory cilia are able to recruit adjacent cilia to beat in a coordinated manner and form a wave, that travels a short distance along the epithelial surface propelling overlying mucus in the same direction.
Periciliary fluid
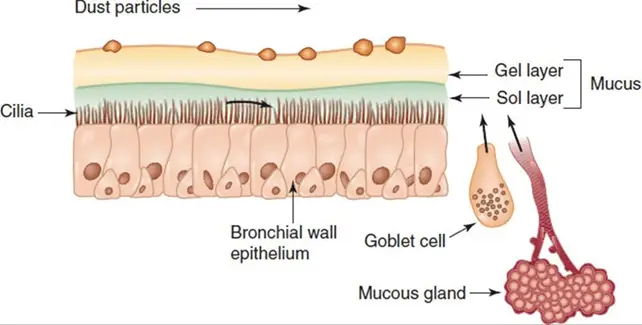
Mucus is moved up stream by cilia but requires a gel layer to effectively slide upon. In healthy lungs, fluid driven by osmotic movement of water from the epithelium and the movement of sodium (Na+) and Chloride (Cl-) ions, is made available to maintain the depth of both the Gel and Sol (liquid) layers (and therefore the efficiency of mucus transport). Periciliary fluid is integral to overcome airway drying from airflow when breathing and without it, mucus would slowly form into plaques, eventually obstructing the airways (Bustamante-Marin & Ostrowski, 2017).
There are many ways that this process can be impacted in the unwell patient or within diseased lungs. The most common impact of acute illness is systemic dehydration which will directly impact the available water for transport into the periciliary fluid. A more specific example would be in the disease Cystic Fibrosis where the CFTR gene responsible for chloride ion flow and the surface level sodium channels are impacted. This leads to considerably thicker sputum (which is harder to transport) and reduced and the periciliary fluid is often reduced impacting mucociliary clearance further (De Rose et al, 2018).
Property of Mucus
Mucus is produced in many types of cells found in the respiratory tree and the prevalence of each the of cell changes depending on how downstream towards the alveoli you travel.
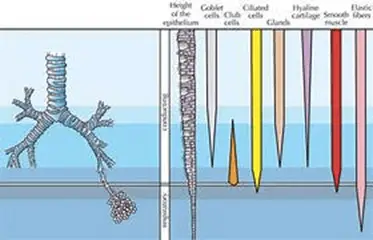
(figure – prevalence of secretory cells within the tracheobronchial tree)
Mucus is composed of salts (1%), water (97.5%) and proteins & glycoproteins (approx 1.5%). One of these glycoproteins is Mucin. Released by goblet cells and reliant on ion concentration in the peri-ciliary region, it absorbs water to maintain lubrication of the ciliated surfaces and is known to attract pathogens aiding in phagocytosis (Hill et al. 2022).
The movement of mucus up the Mucociliary Escalator is impacted by mucous;
- volume
- viscosity
- rheology – specifically mucus elastic properties.
How can we impact the Mucociliary Escalator?
Humidity
As mentioned previously, mucus movement is reliant on adequate fluid in the periciliary layers and this fluid is controlled by ion movement and osmosis in healthy lungs. If a person is particularly dehydrated or they have had dry oxygen applied for a period of time this can drop the volume of available water molecules in the epithelium and the periciliary layers can decrease. Ensuring your patient is systematically well hydrated and choosing humidified oxygen delivery systems can reduce this significantly. Learn more about humidifying patients here: Demystifying Humidification In ICU | Inspire Blog (armstrongmedical.net)
Medication
There are many types of medications that can support in mucociliary clearance – specifically nebulised therapies such as nebulised hypertonic (3, 6 or 7%) or isotonic (0.9%) saline. The former working via osmosis to draw fluid into the gel layer and equally disrupting ion bonds to reduce sputum viscosity (Elkins & Bye. 2011). The latter directly hydrating the epithelium. Nebulised therapy has been advised in many disease guidelines – most recently in the update British Thoracic Society Guidelines for the management of bronchiectasis (BTS 2023).
Another commonly used medication is an oral mucolytic such as carbocysteine which stimulates mucin formation (from secretory glands) and enhances chloride ion transport across the epithelium maintaining and optimising fluid levels in the gel layer and again ensuring maximum airway hydration (Pace et al. 2023).
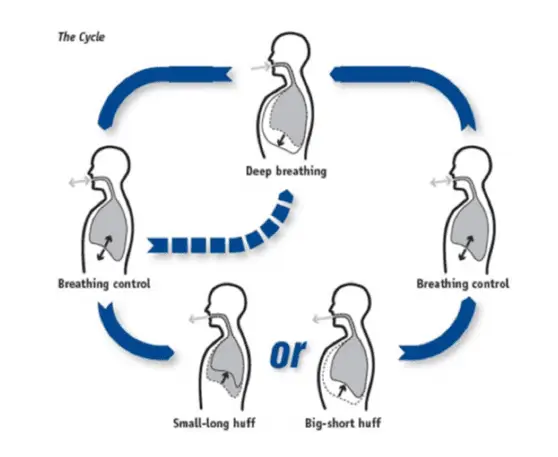
Airway clearance techniques
Physiotherapists have a variety of techniques and adjuncts that work on different aspects of lung physiology and aid the mucociliary escalator. Predominantly these techniques work by altering airway dynamics with a focus on maximising air behind secretions and utilising the 2-phase gas-liquid flow mechanism. This system ensures that the peak expiratory flow (PEFR) always outweighs the peak inspiratory flow (PIFR) supporting the downstream motion of the cilia and propelling mucus towards the upper airway. PEFR must always be a minimum of 10% > PIFR for this to occur (McIlwaine et al 2017).
Complex adjuncts should always be taught by a trained physiotherapist but a simple technique, that anyone can use to support their patients, is the Active Cycle of Breathing Technique.
(Bustamante-Marin & Ostrowski, 2017) – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5378048/
Hill et al. 2022 – https://journals.physiology.org/doi/full/10.1152/physrev.00004.2021
De Rose et al. 2018 : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5911336/
McIlwaine et al. 2017 : https://err.ersjournals.com/content/26/143/160086
Elkins & Bye 2022 : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3128163/
Pace et al 2023 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9227620/
BTS 2023 – https://www.brit-thoracic.org.uk/quality-improvement/guidelines/bronchiectasis-in-adults/
Meet The Author - Holly Hughes
Specialist Respiratory Physiotherapist, Barts Health NHS Trust