The Critical Care Practitioner’s guide to ARDS: traits and treatment
Meet The Blogger
This month’s guest blogger is Jonathan Downham, also known as, The Critical Care Practitioner.
Jonathan is an Advanced Critical Care Practitioner in Birmingham and has worked in Critical Care for over 25 years. He is also an Associate Professor at the University of Warwick teaching on their advanced practice degree. He has a passion for helping others learn about and understand the complex field of critical care.
Jonathan also has many online resources for others to use for their learning at: www.criticalcarepractitioner.co.uk
Acute Respiratory Distress Syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition characterised by rapid onset of widespread inflammation in the lungs. It’s a life-threatening condition that can develop in response to various injuries or illnesses. Here’s a detailed overview:
Characteristics of ARDS:
1. Rapid Onset: ARDS typically develops within a week after the triggering injury or illness.
2.Hypoxemia: One of the hallmark features of ARDS is a significant decrease in blood oxygen levels, leading to difficulty breathing and requiring supplemental oxygen or mechanical ventilation.
3. Bilateral Lung Infiltrates: Chest imaging, such as X-rays or CT scans, will show bilateral (both lungs) opacities or “whiteness” that are not fully explained by effusions, lobar collapse, or nodules.
Causes of ARDS:
- Pneumonia
- Aspiration (inhaling vomit or other substances into the lungs)
- Inhalation of harmful substances (e.g., smoke or chemical fumes)
- Near-drowning
2.Indirect Lung Injuries:
- Sepsis (a severe response to infection)
- Aspiration (inhaling vomit or other substances into the lungs)
- Inhalation of harmful substances (e.g., smoke or chemical fumes)
- Near-drowning
Pathophysiology:
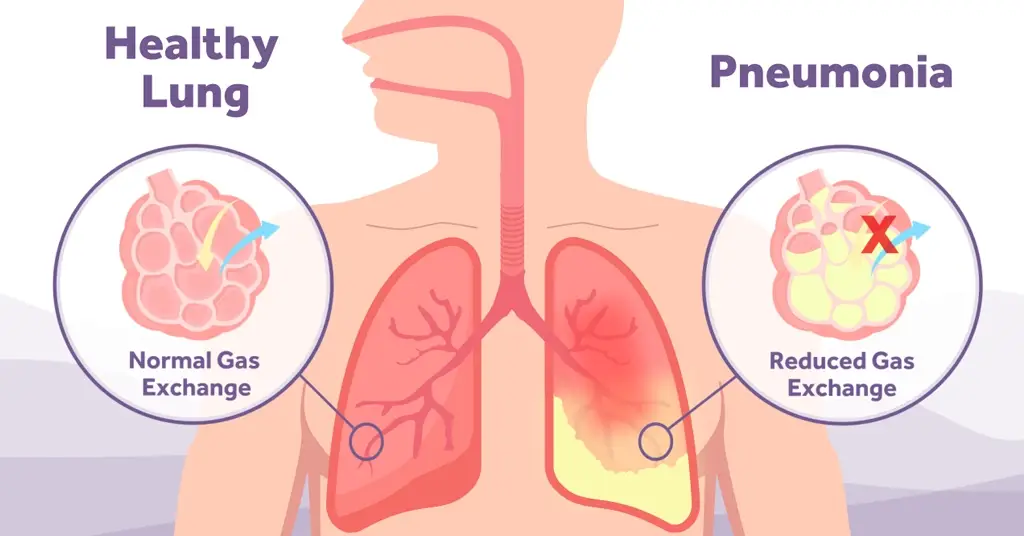
In ARDS, the small blood vessels in the lungs become leaky, allowing fluid to accumulate in the alveoli (tiny air sacs). This fluid prevents the lungs from filling with air, leading to decreased oxygen in the bloodstream.
Symptoms of ARDS:
- Shortness of breath
- Rapid breathing
- Laboured breathing
- Bluish skin or lips (due to low oxygen levels)
- Chest pain or discomfort
- Confusion or drowsiness
Prognosis:
The outcome for people with ARDS can vary. Some people recover fully, while others may have lasting lung damage. The severity of the initial illness, the cause of ARDS, any underlying health conditions, and the quality of care received can all influence the outcome. Mortality rates for ARDS have been reported to range from 30% to 50%, but this can vary based on the population studied and the cause of ARDS.
Mechanical Ventilation for ARDS:
1. Purpose: Mechanical ventilation is used to support or replace the function of the lungs in patients who cannot breathe adequately on their own. In ARDS, the lungs become filled with fluid and inflammatory cells, making it difficult for oxygen to pass into the bloodstream. Mechanical ventilation helps to ensure that adequate oxygen reaches the body’s organs and tissues.
2. Low Tidal Volume Ventilation: One of the key strategies in ventilating ARDS patients is using a low tidal volume, typically around 4-6 ml/kg of predicted body weight. This approach helps to prevent further lung injury by avoiding overdistension of the alveoli (tiny air sacs in the lungs).
3. Positive End-Expiratory Pressure (PEEP): PEEP is the pressure maintained in the lungs at the end of exhalation. In ARDS, higher levels of PEEP are often used to keep the alveoli open, improve oxygenation, and reduce the risk of atelectasis (collapse of the alveoli).
4. Oxygenation Target: The goal is to maintain adequate oxygenation while minimizing potential harm from the ventilator. This often involves accepting lower levels of arterial oxygen than would typically be targeted in patients without ARDS.
5. Monitoring: Patients on mechanical ventilation are closely monitored. This includes regular blood gas analyses to assess oxygenation and ventilation, as well as chest X-rays and other imaging to evaluate lung condition and the position of the endotracheal tube.
6. Potential Complications: Mechanical ventilation is not without risks. Potential complications include ventilator-associated pneumonia, barotrauma (injury due to high pressures), and volutrauma (injury due to high volumes). The goal is to use settings that minimize these risks while providing adequate oxygenation.
7. Weaning: As the patient’s lung function improves, the intensity of mechanical ventilation can be reduced. The process of transitioning a patient off mechanical ventilation is called weaning. This is done gradually, ensuring the patient can breathe adequately on their own without the support of the ventilator.
Prone Positioning in ARDS:
Purpose: Prone positioning involves placing a patient face-down. This position can improve oxygenation in patients with ARDS by optimizing the distribution of air and blood in the lungs.
Mechanisms of Benefit:
1. Improved Ventilation-Perfusion (V/Q) Matching: In ARDS, the posterior (back) parts of the lungs often have more damage and fluid accumulation. When a patient is supine (on their back), these areas receive more blood flow but are poorly ventilated, leading to V/Q mismatch. Prone positioning redistributes blood flow to better-ventilated areas of the lung, improving oxygenation.
2. Alveolar Recruitment: Prone positioning can help open up collapsed alveoli, increasing the functional lung volume.
3. Reduced Lung Compression: The heart’s weight can compress the lungs when a patient is supine. Prone positioning reduces this compression, especially in the posterior lung regions.
4. Improved Secretion Drainage: Being in a prone position can facilitate the drainage of secretions from the lungs.
Duration:
Patients may be kept in the prone position for extended periods, often 12-16 hours at a time, followed by a period in the supine position.
The decision on how long to keep a patient prone and how often to turn them is based on the patient’s oxygenation response and other clinical factors.
Potential Complications:
1. Pressure Sores: Extended periods in one position can lead to pressure sores or ulcers, especially on the face and bony prominences.
2. Dislodgement of Lines and Tubes: There’s a risk of dislodging medical equipment like endotracheal tubes, central lines, or arterial lines during the turning process.
3. Facial Edema: Prolonged prone positioning can lead to fluid accumulation in the face.
4. Eye Injuries: The eyes need to be protected to prevent injuries or pressure-related complications.
Evidence:
Multiple clinical trials and observational studies have shown that prone positioning can improve oxygenation in ARDS patients. Some studies have also demonstrated a mortality benefit in patients with severe ARDS.
Considerations:
Not all ARDS patients will benefit from prone positioning. The decision to use this intervention is based on the severity of hypoxemia, the underlying cause of ARDS, and other patient-specific factors. It’s also crucial to consider potential contraindications, such as spinal instability or recent abdominal surgery.
Summary
With all the experiences we had during COVID we became much better at, and more willing to prone our patients who had very similar lungs to those suffering with ARDS. The evidence would seem to suggest that it does make a difference, but it’s also important to remember the other interventions we can make to supplement this. From my experience lung protective ventilation is also crucial and relatively easy to do with today’s modern ventilators.
So remember to always look at those tidal volumes and if you have to, prone early.
ARDS Definition Task Force, Ranieri, V. M., Rubenfeld, G. D., Thompson, B. T., Ferguson, N. D., Caldwell, E., Fan, E., Camporota, L., & Slutsky, A. S. (2012). Acute Respiratory Distress Syndrome. JAMA, 307(23), 2526–2533. https://doi.org/10.1001/jama.2012.5669
Gattinoni, L., Taccone, P., Carlesso, E., & Marini, J. J. (n.d.). Concise Clinical Review Prone Position in Acute Respiratory Distress Syndrome Rationale, Indications, and Limits. https://doi.org/10.1164/rccm.201308-1532CI
Griffiths, M., & Baudouin, S. (2018). GUIDELINES ON THE MANAGEMENT OF ACUTE RESPIRATORY DISTRESS SYNDROME. https://www.ficm.ac.uk/sites/default/files/ficm_ics_ards_guideline_-_july_2018.pdf
Guérin, C., Reignier, J., Richard, J.-C., Beuret, P., Gacouin, A., Boulain, T., Mercier, E., Badet, M., Mercat, A., Baudin, O., Clavel, M., Chatellier, D., Jaber, S., Rosselli, S., Mancebo, J., Sirodot, M., Hilbert, G., Bengler, C., Richecoeur, J., … Ayzac, L. (2013). Prone positioning in severe acute respiratory distress syndrome. The New England Journal of Medicine, 368(23), 2159–2168. https://doi.org/10.1056/NEJMoa1214103
Tanaka, L. M. S., Azevedo, L. C. P., Park, M., Schettino, G., Nassar, A. P., Réa-Neto, A., Tannous, L., de Souza-Dantas, V. C., Torelly, A., Lisboa, T., Piras, C., Carvalho, F. B., de Oliveira Maia, M., Giannini, F. P., Machado, F. R., Dal-Pizzol, F., de Carvalho, A. G. R., Dos Santos, R. B., Tierno, P. F. G. M. M., … Salluh, J. I. F. (2014). Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Critical Care (London, England), 18(4), R156. https://doi.org/10.1186/cc13995