Demystifying humidification in ICU

With such a busy environment in our Healthcare system, so many new staff and immense pressure on resources; saving time and cost are of the essence.
Humidifying patients can be a confusing phenomenon; learning how it works, when to apply it and what works best for each patient, alongside grasping the medical equipment needed for the treatment.
Let us explore humidification.
For both ventilated and non-invasive ventilated patients there are two options: active or passive humidification.
Absolute Humidity and Relative Humidity
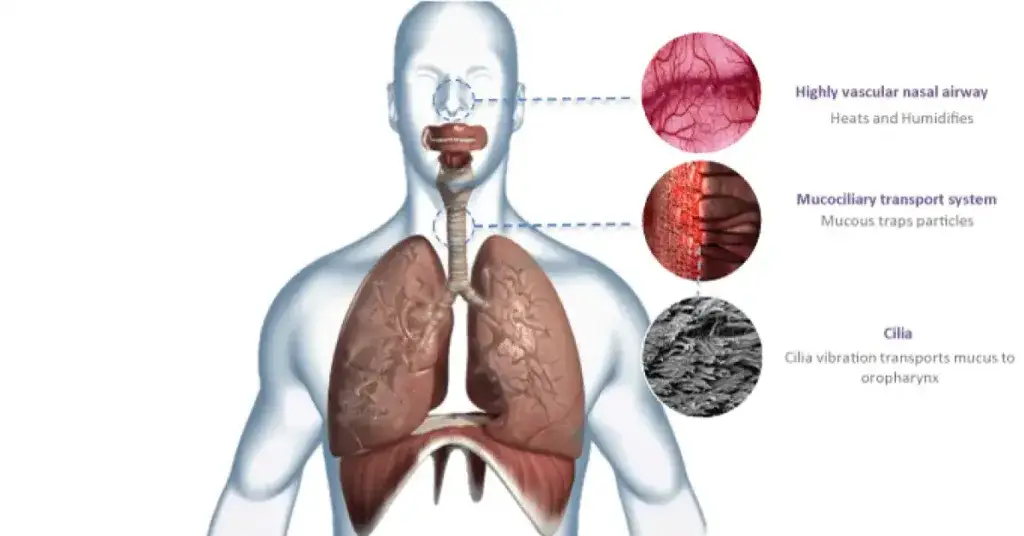
Our natural ability to humidify
What happens when we artificially ventilate a patient?
Passive humidifcation - HMEs
Active Humidification
Choosing Active or Passive Humidifcation?
We know that decisions regarding active or passive humidification will remain on the cards for many years to come but it is important to remember the fundamental benefits of delivering humidification (in whatever method) to patients requiring respiratory support.
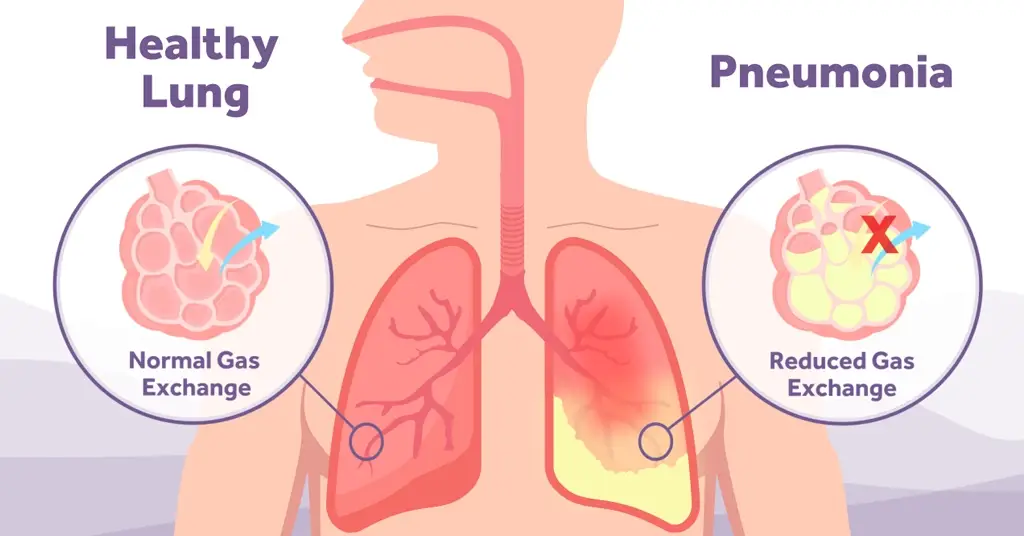
If we look at the anatomy of our bodies, and in particular our lungs, performing all the wonderful jobs they are designed to do; they are truly amazing.