Fluid filled lungs; causes and treatment

Non-invasive positive airway pressure therapy is used extensively in healthcare to support patients with varying lung morbidities causing infections such as pneumonias and Covid 19; being the most recent.
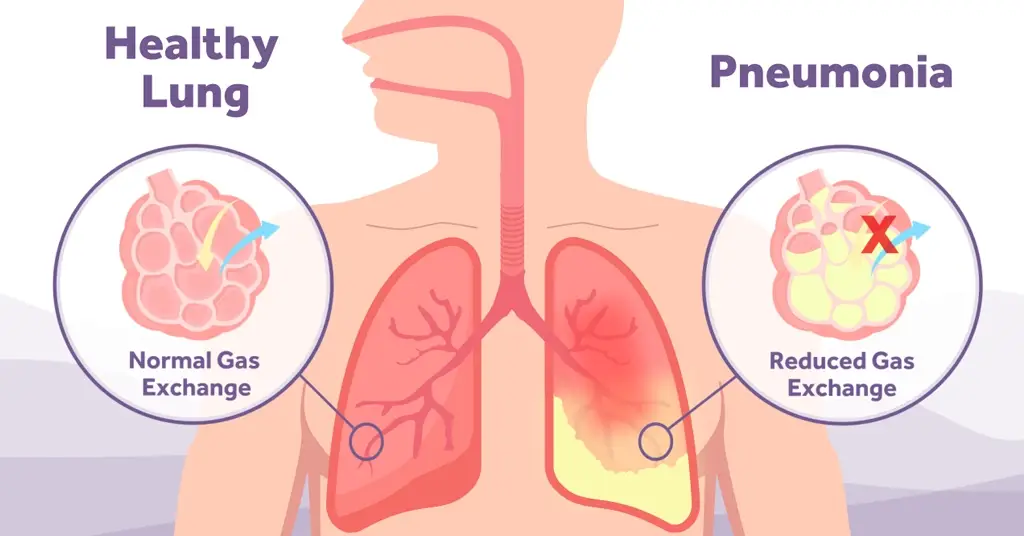
These infections can result in the lungs filling with fluid which will always have serious implications for the patient if not treated quickly.
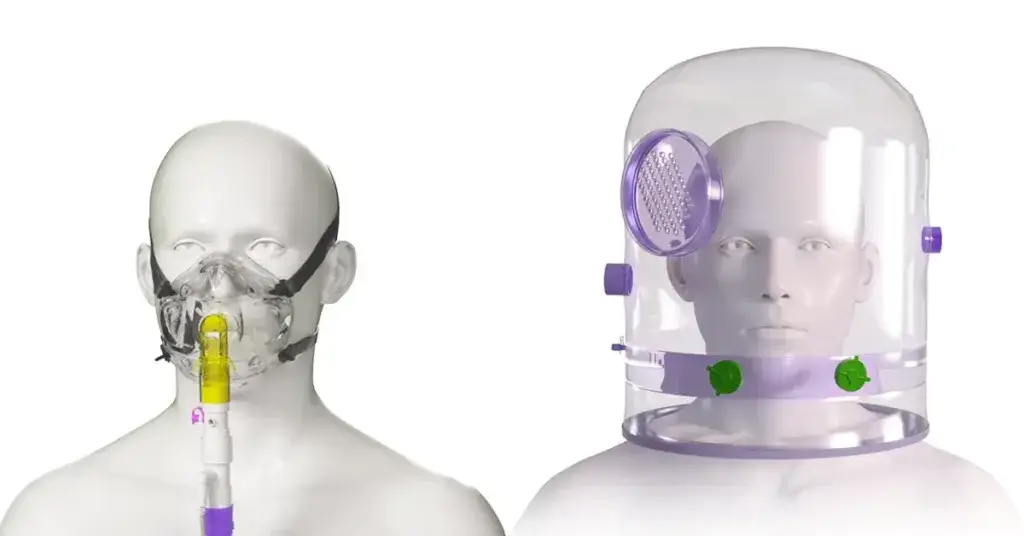
One non-invasive positive airway pressure therapy to treat fluid-filled lungs is Continuous Positive Airway Pressure (CPAP) which can rapidly improve blood gas exchange, work of breathing and associated breathlessness in lung sick patients [1]. CPAP delivers a constant flow of air/O2 and generates a continuous level of positive distending pressure to the patient’s airways. This distending pressure, or PEEP effect, works to open the airways and ensure that the lungs don’t collapse at the end of an expiratory breath. Additionally, for patients experiencing collapse in the terminal bronchioles and alveoli, positive pressure delivered by CPAP works to re–inflate or ‘re-recruit’ these areas, optimising surface area for gaseous exchange [2].
Fluid Filled Lungs/Pulmonary Oedema
Another common respiratory problem that CPAP can be used to treat is conditions that cause fluid build-up within the lungs themselves. Known as Pulmonary Oedema, this fluid accumulation puts considerable strain on the patient’s body resulting in symptoms such as shortness of breath, coughing up of blood, wheezing, chest pain and increased heart rate. CPAP works to re-recruit the areas of lung tissue that cannot participate in gaseous exchange due to the presence of the fluid [2]. The distending positive pressure provided by CPAP therapy aids the movement of fluid out of the lung tissue into the blood stream and lymphatic system.
In patients suffering from Pulmonary Oedema the primary aim is to support vital functions such as breathing and heart rate, before treating the underlying condition and cause. CPAP can be used to relieve the burden of the fluid in the lungs and begin to decrease the fluid build-up. At the same time clinicians will use medications and other treatments to aid this process as well as treat the underlying cause. Unfortunately, CPAP is a treatment and not a cure.

Conditions that lead to a fluid filled lung
Pulmonary Oedema can be the result of any of the following conditions or problems, although this list is not exhaustive.
Type 1 respiratory failure such as Acute Respiratory Distress Syndrome (ARDS)
This syndrome was first described as ‘an acute inflammatory syndrome manifesting as diffuse pulmonary oedema and respiratory failure that cannot be explained by, but may co-exist with, left-sided heart failure’ [3] by the American-European Consensus Conference on ARDS. Alterations to this definition have been made since, recognising three levels of severity depending on the degree of hypoxaemia and including the application of at least 5 cmH2O of PEEP or CPAP [4,5].
Heart Failure
A patient experiencing heart failure cannot pump enough blood, and therefore oxygen, around their body to support vital organs. Resulting in fluid build-up in the lungs due to the backup of pressure in the blood capillaries found in lung tissue. This increase in pressure found in these capillaries causes the vessels to leak fluid from the bloodstream into the alveoli.
Kidney Failure
The inability to excrete fluid from the body resulting from kidney failure can cause fluid to build-up in the blood vessels. This excess fluid needs to go somewhere and often ‘leaks’ into the lungs resulting in pulmonary oedema. While CPAP may be used to help rid the lungs of fluid patients, advanced kidney disease may require dialysis in conjunction with CPAP to ensure excess body fluid is removed.
Treatment of pulmonary oedema can be complex, with a multi-prong treatment option often offered to combat the problem. In patients where CPAP is utilised to reduce the amount of fluid found in the alveoli, an easy-to-use CPAP delivery system may be useful to aid clinicians in their therapy delivery and subsequent weaning from respiratory support for the patient.