On International Women’s Equality Day, and every day, we celebrate women doing an amazing job in healthcare all over the world.
This year we want to shine a light on an all-female team making a difference to the babies in their care.
Embracing rapid change and development leading to “Project PEEP”
At University Hospitals Coventry and Warwickshire staff have been embracing a period of rapid change and development, with a new clinical lead and new consultants joining the team. Dr Nitesh Singh, who is one of the consultants, along with Dr Sarah Williamson (ST7), introduced a Quality Improvement (QI) Initiative. Both, medical and nursing staff, were divided into teams and challenged to complete a QI project.

Team Members
The team for “Project PEEP” consists of 6 enthusiastic interdisciplinary members, Advanced Nurse Practitioner Lucy Bradley who is leading the project alongside Dr Teim Eyo (ST2), Zara Grandison – Neonatal co-ordinator, Jo Jones – Neonatal sister, Jay Carter – Neonatal Sister and Yvonne Huskins – Practice Educator.
The team is passionate about reducing the incidence of Bronchopulmonary dysplasia within their level 3 neonatal unit, and we at Armstrong Medical were proud to support the team entering the competition at this year’s REaSoN Neonatal Conference.
Developing a preterm respiratory care practice bundle
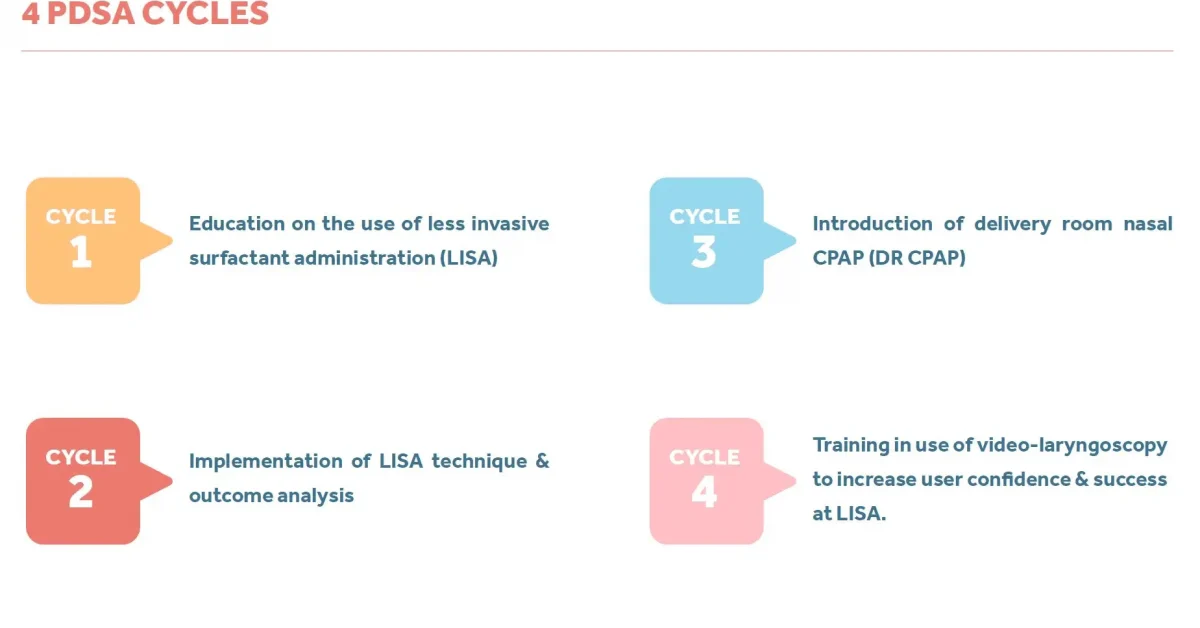
Through successful implementation of QI methodology, the team has developed a preterm respiratory care practice bundle, and over a period of 4 “Plan-Do-Study-Act” cycles they were able to introduce a number of practice changes.
The team provided education and training in relation to factors which may influence BPD:
4 cycles v2
promoting the use of non-invasive ventilation
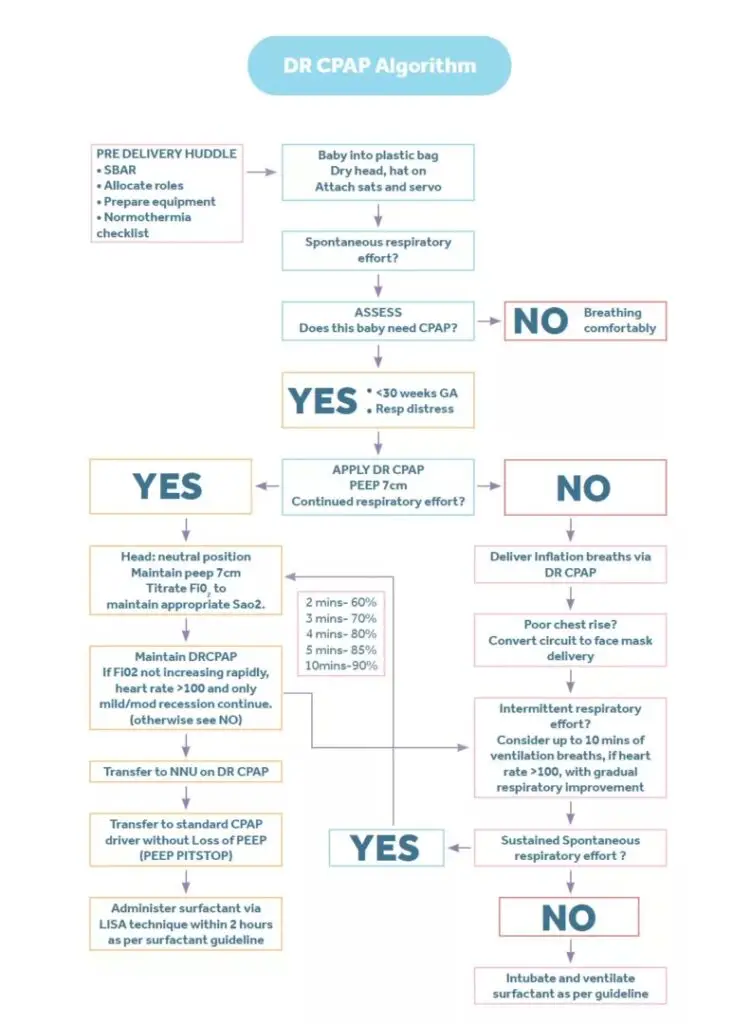
creating strategies to reduce the need for intubation in the delivery room through the use of Delivery Room CPAP (DRCPAP) and
facilitating the application of less invasive surfactant administration (LISA) through education and training in the technique
Delivery Room CPAP
Each team member trained a group of staff of equivalent grading, which was supported by a 2-minute video tutorial filmed by the QI team featuring Jo. DRCPAP has quickly become an accepted and well embedded practice within the unit, with the QI team acting as champions, facilitators and problem solvers where necessary.
Less invasive surfactant administration (LISA)
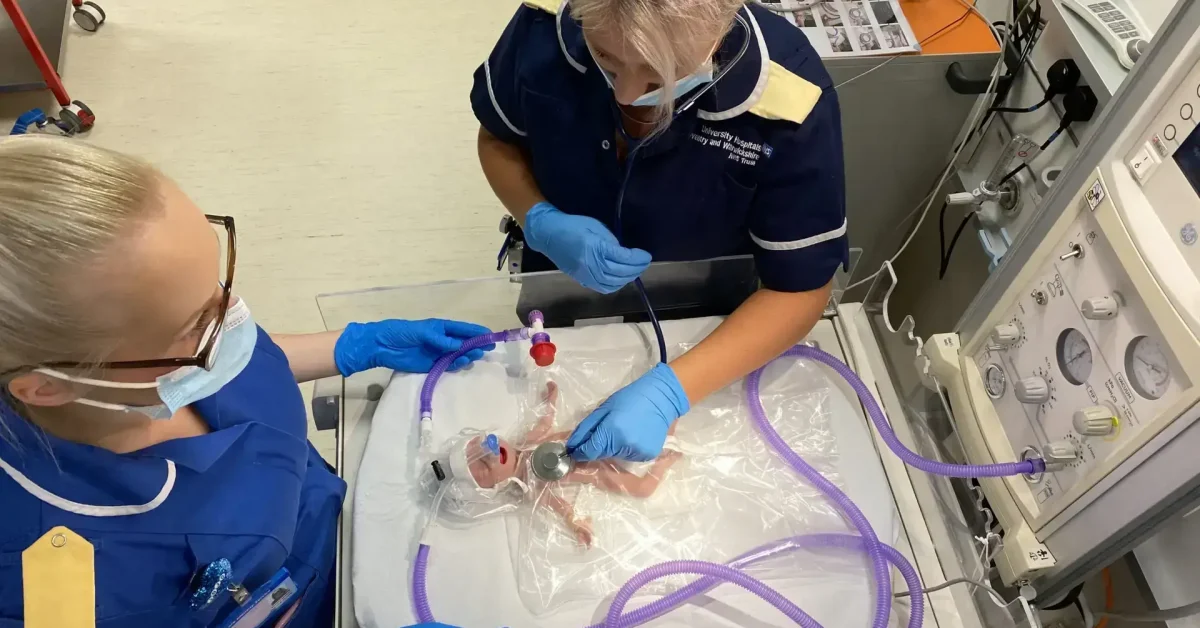
With the avoidance of intubation at delivery, LISA has become increasingly adopted and the unit has now performed LISA in excess of 80 times at UHCW, with the smallest baby to have received surfactant in this way weighing 635grams. The QI team believed a video laryngoscope would increase whole team confidence and skill at this technique and so successfully applied for and was granted charitable funds to purchase one. Training has been completed and the QI team anticipates the application of the practice bundle at smaller weights and gestations because of this.
Summary
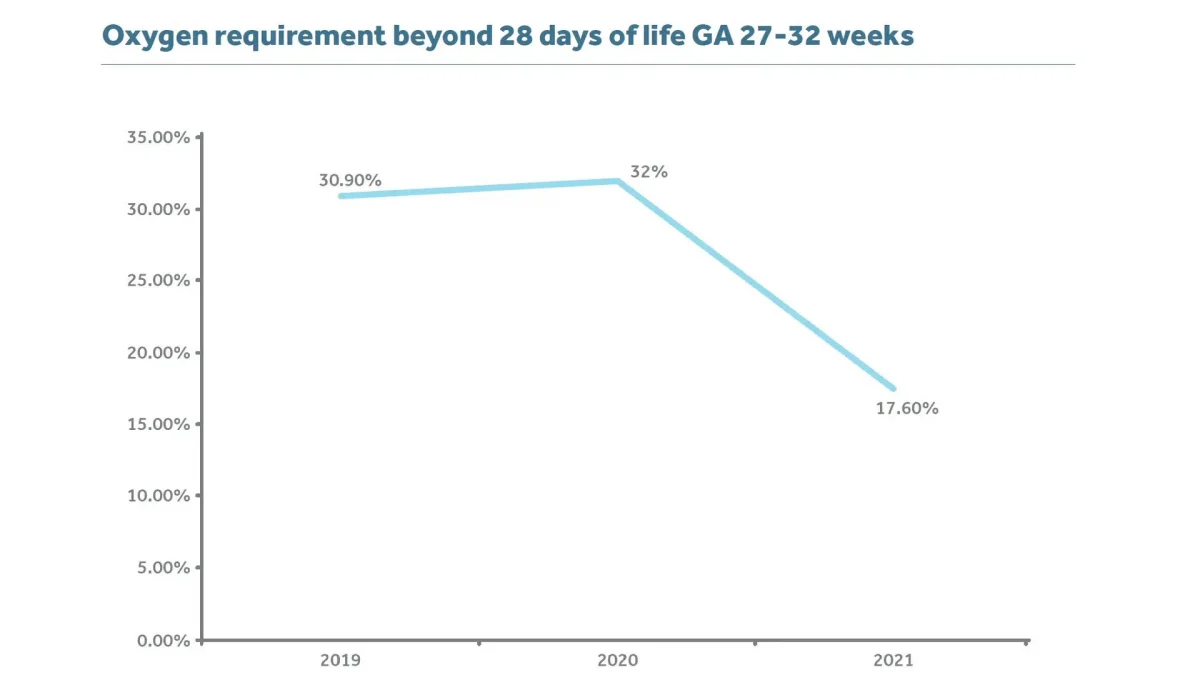
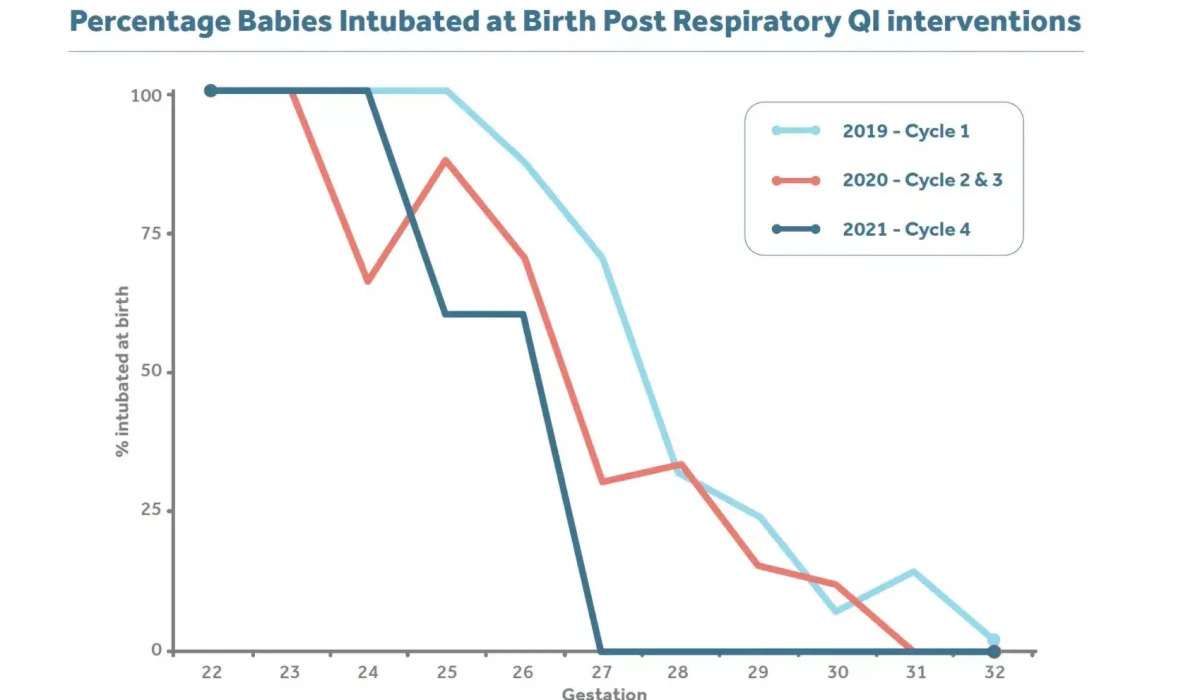
As a result of the practice bundle, they have seen a reduction in delivery room intubations between the gestation 27-32 weeks from 70% in 2019 to 0% at time of analysis 2021. They have also seen the number of babies requiring oxygen at 28 days fall significantly from 32% to 17.6%, which they hope will positively influence their rates of BPD in the future.
Celebrating the team on Women’s Equality Day
On Women’s Equality Day we would like to applaud the ‘Project PEEP’ team members Lucy, Dr Teim, Zara, Jo, Jay and Yvonne from the NICU at University Hospital Coventry, who won this year’s Quality improvement Session at the REaSoN Neonatal Conference. The collaboration of the Project Peep team has produced a fantastic Quality Improvement Initiative to improve respiratory outcomes for their premature patients.
Lucy describes the team’s pride:
“As an all-female QI team, we are exceptionally proud of the work we have achieved and are excited to continue with more change ideas and further develop the practices already implemented.”

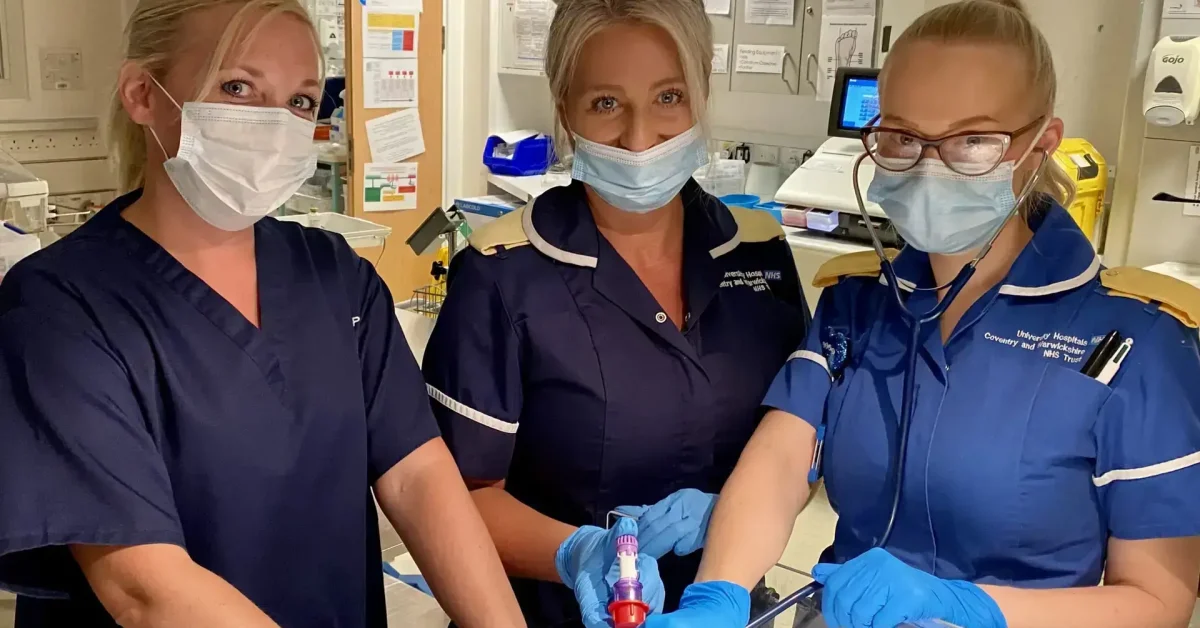
From left to right: Dr Teim Eyo, Lucy Bradley, Zara Grandison, Jo Jones
Each of the female team members has had a crucial role to play in the successful implementation of the practice changes. The team approach to training and education of Delivery Room CPAP was especially important as it achieved a much greater influence over negative cultural opinions and resistance to change, than one individual would ever be able to achieve.
The team shares their female inspirations:
“We have multiple women who inspire us but Lucy is particularly inspired by Dr Sarah Williamson who has motivated UHCW to make positive quality improvement changes through the introduction of this challenge with Dr Singh and by her own example of the many projects she has completed.
Zara is inspired by her mum whose strength and determination has enabled her to overcome adversity and be the poised and confident woman she is today. Dr Eyo is inspired by Inye Boyle, her mum, whose exemplary life of service to others and strong faith continues to fuel her determination to daily be a better version of herself.