The highs and lows of the ROX index

With the increased use of high flow oxygen therapy (HFOT) in the critical care space and on respiratory wards, a measure of its use is vital for the clinician to be able to check success, failure or, more importantly, the predictability of both.
The ROX index (Respiratory rate and OXygenation) gives an indication of who is going to succeed or fail on HFOT and by doing so identify those who will need to escalate to mechanical ventilation, if failure is predicted. Not only does the prediction of HFOT failure in patients with acute hypoxemic respiratory failure improve clinical management and stratification of patients for optimal treatment [4], it can aid hospital workflow and bed management, as well as ensuring patient safety throughout their treatment.
Getting the whole picture
The fact that there is a single, easy to calculate index looking at all these combined could aid the clinician to organise patients rather than wait to reach a stage where it is simply too late to intubate or escalate treatment. There is a downside to waiting too long to intubate a patient, which is why the ROX index was designed to help determine whether the patient is safe or should be intubated. [5]
The concept
This was calculated on a set of patients receiving a minimum of 30L of flow and 100% FiO2. They were aiming for O2 saturations > 92%. The study also found that the median duration of those who did well on HFOT was three days and those who did not do well, tolerated HFOT for about one day.
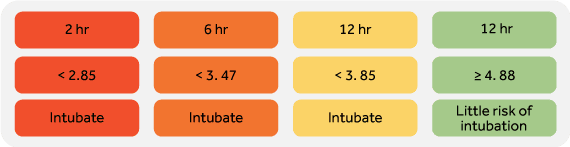
After Roca et al. carried out this study, they looked at the ROX index again and in 2019, carried out a prospective observational cohort study over 2 years this time[6]. The authors found that a ROX less than 2.85, less than 3.47, and less than 3.85 at 2, 6, and 12 hours of HFOT initiation respectively, were predictors of HFOT failure and that the ROX index was better than looking at SpO2/FiO2, RR, PaCO2, flow, SpO2, FiO2, and lactate to predict the need for mechanical ventilation; cementing further the need to use such an index.
The calculation
Given that it is possible that HFOT failure could delay intubation and increase mortality [5], it is mandatory for these patients to be monitored in specifically designed physical spaces such as Respiratory Intermediate Care Units or the ICU, where healthcare personnel safety can also be optimised. [2]
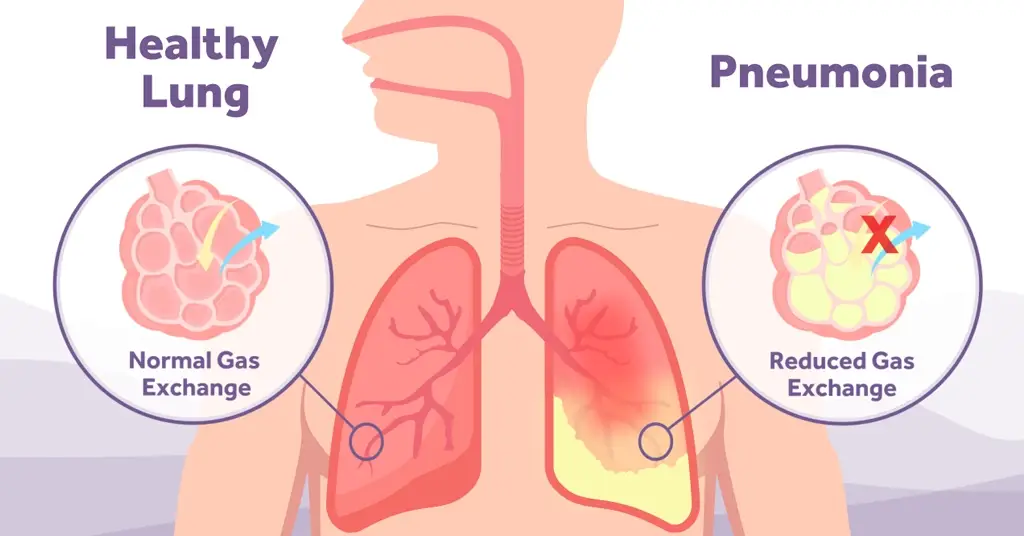
What is HFOT?
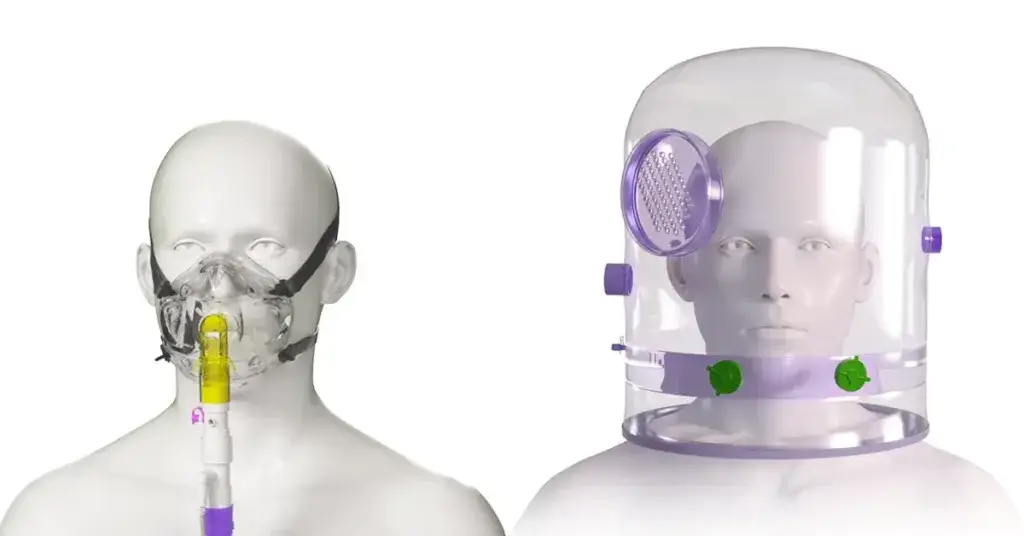
HFOT is a well tolerated and comfortable, humidified non-invasive oxygen therapy delivering high flow rates of up to 80 l/min (depending on device) via nasal prongs. Delivering 37°c of flow with oxygen to deliver optimum comfort and humidification to the patient, the flow rates should be delivered and calculated based on patients’ inspiratory demand which HFNO should exceed.
- Improves oxygenation due to decreased O2 dilution and therefore delivering a stable fraction of inspired oxygen to the alveoli. This is particularly true in patients with high minute volumes where the risk of entraining added room air is more likely
- Enhanced dead space washout
- Mucociliary clearance due to the use of humidification- airway dehydration is reduced, and secretion clearing is increased
- Varied PEEP
- Reduced work of breathing – a study demonstrated that compared with low oxygen flow, HFOT and NIV both reduce the respiratory muscle load on the respiratory system, resulting in a change in breathing pattern and reducing respiratory rate.[3]
HFOT can be used for break and weaning from CPAP as well as a standalone treatment. It can be used in ED, throughout acute respiratory wards, and through to critical care as necessary. It also has a growing space within the pre, peri and post operative space in theatres (respiratory support during procedural sedation, tubeless field surgery, obstetric anaesthesia and airway management in obese patients and difficult airway management) with the use of our Armstrong POINT system.
[1] Roca O, Messika J, Caralt B, García-de-Acilu M, Sztrymf B, Ricard JD, Masclans JR. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016 Oct;35:200-5.
[5] ROX Index: Predicting Who Is or Isn’t Going to Fly on HFNC (eddyjoemd.com)